Today, an overtired, actively involved mother of a child with speech and feeding problems due to motor dysfunction was pondering why more parents do not seek out the services of therapist like me and my team for their children. This mom searched and searched until she found someone who understood how her child’s motor dysfunction was negatively impacting her oral development, speech, and feeding skills. Her questions were gut wrenching because we only met a few months before her child’s 3rd birthday.
As the mom and I were talking, she described to me what she told the school district her plans were for her child given her upcoming admittance to preschool. Her child will be discharged from early intervention soon as she is turning three. She said “Well, I told them I have “myo” and feeding, then they will do speech at school.” Now, she has used the word “myo” before to talk about my therapy and to my regret today, I have not corrected her. In her research for treatment to improve her child’s oral motor dysfunction and I am guessing from her early intervention speech therapist; she assumed her daughter needed myofunctional therapy. I apologized for not better explaining the underlying theoretical position of my therapy and providing a description of the speech and feeding goals that drive my therapeutic activities and strategies.
What was I doing? Mostly feeding therapy, but I was also using strategies from PROMPT, OPT, and other speech producing strategies to target the CVCV combos in the Kaufman speech to Language Set Treatment Kit 1. The feeding therapy strategies were targeting jaw endurance (also called grading), tongue/jaw dissociation, tongue retraction and tongue tip control. The speech strategies I was implementing were targeting jaw grading using rhythmical jaw movements, improving production of the VMS /p,b/ and the /m/ sounds, and at the same time using simple sound combinations to form word approximations in imitation to develop a word template to improve vocabulary development. This is not Myofunctional therapy, my goals are targeting speech and feeding. While the therapy activities may appear similar to those used in myofunctional therapy if one is unfamiliar with it, the goals I have for this child are to improve speech and feeding skills and as a speech and language pathologist, those are the skills I am licensed to treat.
This is not the first time a parent has come to my office with a preschool age child and asked for myofunctional therapy. It seems there is a misunderstanding in the difference between oral motor dysfunction in children and orofacial dysfunction causing myofunctional problems. There is a lot of chatter in social media groups about myofunctional therapy and tongue ties. When a parent of a child who has problems with speech or feeding reads this information in groups of parents, the types of therapy can sound similar, and it can be confusing. It is true that speech and feeding therapy as well as myofunctional therapy require improved muscle function of the oral motor structures, but there are distinct differences in the treatment and who can provide the treatment.
Given the increase in folks discussing and seeking therapy to improve oral function related to things like airway issues, sleep disordered breathing, and tongue tie, there is a bit of confusion on the different types of therapy for improving oral functioning. Many dental professionals who discuss with their patients needing oral motor therapy may call it OMT (oral motor therapy or oral myofunctional therapy). In many cases, a patient may need therapeutic intervention to improve the function of their oral motor structures either before or after dental treatment (including orthodontic work) or pre and post therapeutic intervention for oral motor dysfunction related to tongue and lip restrictions. The term OMT is difficult and can be confusing because it also means Osteopathic Manipulative Treatment, which is also sometimes recommended for those struggling with orofacial problems. In the next few sections I will discuss the different types of therapy that address oral motor dysfunction in some detail. My goal is to provide explanations to help guide those seeking treatment. Proper understanding can help those in need access the care and not waste time and money trying to find the appropriate therapy. Patients and parents of patients are their own best advocates and this information will level the playing field for those who are not sure what type of therapy they or their child need.
Myofunctional Therapy
I think it is best to start with myofunctional therapy, since in my experience this is the term most parents of children with oral motor dysfunction use. It is also a hot topic in circles focused on airway health and sleep apnea. Myofunctional therapy provides an exercise training program for the muscles around your face, including the mouth and tongue when there is a presentation of an orofacial myofunctional disorder. According to WebMD this is the definition of an orofacial myofunctional disorder:
Orofacial myofunctional disorders (OMD). OMDs are characterized by an abnormal pattern of facial muscle use. OMD interferes with how the facial muscles, including the tongue, are used. People who suffer from OMD might also struggle to breathe through their nose.
Myofunctional therapy for orofacial myofunctional disorders is becoming more popular as research is beginning to emerge that demonstrates that this type of therapy improves speech, feeding, breathing, and in some patients may improve sleep apnea symptoms. The exercises provided during myofunctional therapy usually include normal oral resting posture where the teeth are together, not clenched, tongue is resting in the roof of the mouth, lips are sealed and there is nasal breathing. The exercise program may include activities for tongue tip resting posture, lip closure, and nasal hygiene. Myofunctional therapy can be done by speech pathologists, registered dental hygienists, and any medical provider that has been trained by an accredited program. There is no license for myofunctional therapy because it is a treatment modality, and it is not covered by insurance. It is most common that an adult or child will be identified as having a myofunctional disorder during a routine dental exam.
Feeding Therapy
Feeding therapy focuses on improving swallow functioning. There are several stages of the swallow that begin with the oral phase. The oral phase of the swallow is the process of taking a bite, chewing the food, getting the food ready to be swallowed, and it ends with the initiation of the swallow. Once the swallow is initiated, this triggers the second phase of the swallow called the pharyngeal phase. The only phase of the swallow that can be improved by the therapeutic interventions of a speech and language pathologist is the oral phase. While improvements in the oral phases of the swallow can improve the pharyngeal phase, there are no direct treatments. To start feeding therapy, there needs to be a full oral motor feeding evaluation. During this evaluation, the speech and language pathologist will evaluate what the oral motor structures are doing at each stage of the oral phase of the swallow. In my office we use the Beckman Oral Motor Protocol, a modified oral motor evaluation from the SMILE program, as well as an orofacial protocol from the IAOM. The patient is also observed eating a variety of textures and drinking from containers and straws. All of the information obtained during the feeding evaluation is used by the speech and language pathologist to create a treatment plan that includes long term goals and short-term objectives. The focus of the treatment plan is improving the part or parts of the oral phase of the swallow that are dysfunctional.
During feeding therapy, the speech and language pathologist uses therapeutic strategies to improve the function of jaw, lips, and/or tongue for swallow function. This may include oral motor exercise in the absence of food if the patient is at risk for choking or aspiration with difficult to chew foods. Impairment of any part of the oral phase of the swallow can put the patient at risk of both choking and aspiration. Speech and language pathologists with experience in feeding are trained to identify these risks and to modify what and how someone is eating to reduce these risks as much as possible. The long-term goal of feeding therapy is to improve oral motor functioning for age-appropriate safe oral intake of daily nutrition. Our therapists use a variety of methodologies to target deficits, there is no one program that is suffice. Feeding problems are often complex and require a variety of therapeutic techniques for skill improvement. This may include therapeutic activities similar to those used for myofunctional therapy, but the difference is in feeding therapy the focus in on improving swallowing.
In some cases, patients have noted improvements in speech production while working on feeding therapy, especially young children struggling with speech production. While the activation and control of the oral motor muscles is different for speech and feeding, the target movement can help overall orofacial functioning.
Speech Therapy
When there is a speech production problem, an evaluation by a speech and language pathologist is necessary to determine the production errors and how these errors are impacting overall speech production. Speech sound productions are evaluated at the word and sentence level. An informal language sample is also utilized to evaluate intelligibility and fluency in a natural speech sample. In our practice, we use the Goldman Fristoe Test of Articulation Third Edition to test the speech sounds. If a child is minimally verbal or has a small vocabulary, we will use the Kaufman Praxis Test to test sound productions in imitation. The results from both the articulation testing and language sample are used to determine if there is a production problem and if there is, the speech and language pathologist will determine the level of severity.
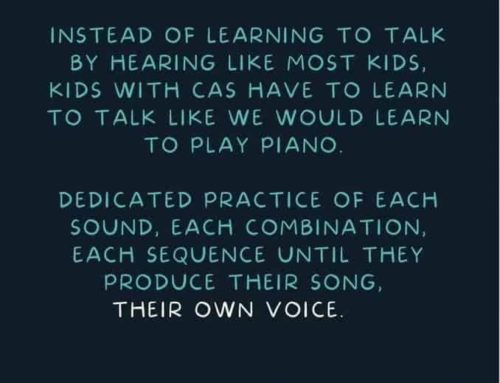
Speech therapy includes therapeutic intervention that helps improve the production of speech sounds in isolation, in words, phrases, sentences and then finally in conversational speech. Speech production problems include respiratory control, phonatory control, jaw movements, lip movements, and tongue movements. For intelligible speech, a person must coordinate body parts from the diaphragm to the lips. It has been said that it takes over 70 body parts to produce a single syllable word. During speech therapy, the speech and language pathologist targets deficit areas and provides activities and strategies for improved production. The results from articulation testing are used to create a treatment plan with the long-term goal of articulation therapy being to improve speech production skills to age-appropriate levels. Our therapists use a variety of techniques including the Kaufman speech to language kits, OPT, and traditional methods to address articulation problems. Like with feeding, each patient has an individualized plan based on their evaluation, while the long-term goal remains the same, the actual treatment varies patient to patient.
Summing up the Differences
There is a clear difference in the type of treatment necessary for those requiring oral motor therapy. Therapies for myofunctional, feeding, and speech disorders all require some improvement oral motor functioning, but their evaluation and treatment are distinctly different. Myofunctional therapy is an exercise program to improve muscle function, speech and feeding therapy provides specific treatment plans to improve specific impairment of speech and feeding skills that are negatively affecting function. Myofunctional therapy can be provided by a variety of practitioners without specific licensure. Speech and feeding therapy must be provided by a licensed speech and language pathologist who has specialized training. Myofunctional therapy is specific to those patients with orofacial myofunctional disorders while speech and feeding therapy targets the deficits in the oral motor skills necessary for speech and feeding function. Speech and feeding therapy can be appropriate for those with orofacial myofunctional disorders when there is an impact on how they produce speech and/or and swallow.
Unlike myofunctional therapy, both speech and feeding therapy can be provided to young children who do not have the cognitive ability to follow complex directions. Myofunctional therapy requires patients to understand what is being asked of them and to complete those activities because it is an exercise program. A speech and language pathologist can provide therapeutic strategies that encourage the appropriate movements of the oral motor mechanism for both speech and feeding without complex directions or tasks. For this reason, many practitioners encourage myofunctional therapy to begin around 7 years of age. Feeding therapy can begin at birth if there is trouble with breast or bottle feeding and speech therapy can begin as soon as there are signs of a speech production disorder.
Conclusion
Most of the patients that are referred to my office as a speech and language pathologist for myofunctional therapy, swallow with their tongue pushing on or through their teeth. These patients are either in orthodontics or need them and the orthodontic provider will not take them off or put them on until the child’s swallow improves, This, however, becomes a feeding problem and requires feeding therapy, which is why there were referred to a speech and language pathologist. Many times, these patients also have speech production problems where the placement of the articulators during speech is incorrect and requires specific speech therapy interventions.
When infants and toddlers come in with feeding problems, many times medical clearance from other providers like an ENT or GI is necessary before any therapy can begin. The same is true for toddlers and young children referred for speech, especially when they present with open mouth posture and mouth breathing. Even teenagers with speech or feeding problems may require additional medical intervention, including dental or orthodontic treatment, before therapy can be implemented. Feeding problems and speech problems can be very complex and sometimes they are just one of the symptoms of another problem.
Steps for those in needs
With the increase in discussion of orofacial myofunctional disorders and their negative impact on speech and feeding function, it is important to have a full understanding of the complexity of the topics being discussed. It is also important that individuals and parents understand the difference in the type of therapies available so they can seek the most appropriate therapy for their needs.
It is becoming more common for medical professionals to identify oral motor dysfunction in young children. Pediatricians may be concerned with poor height and weight gains, prolonged bottle or pacifier use, or they may notice a child is very difficult to understand or not use enough words for their age. Dental professionals may identify poor oral resting posture, orofacial abnormalities from thumb and pacifier use, or teeth wearing from grinding or clenching. All these early problems can lead to dental and medical problems as the child grows and develops. The oral motor problems identified in young children are best treated by a speech and language pathologist who understands oral motor and feeding development. An evaluation from a speech and language pathologist can help identify oral motor problems and provide treatment to help improve the function of the oral motor mechanism for both speech and feeding. The evaluating therapist can also identify whether the child presents with motor, sensory, or medical issues and make the appropriate medical referrals.
Some examples may help with understanding the complexity of speech and feeding problems. Something we see often in my practice is a referral for poor oral resting posture. Often, during an initial evaluation, the therapist comes to realize that the child is having problems related to sleep or breathing. This child would be referred to an ENT (Ears, nose, and throat) for evaluation of the airway. The therapist may also notice that the child has a hard time sitting up and taking deep breaths, the therapist would likely make physical therapy referral to determine the effect these problems are having on the child’s functioning. The therapist may also notice the child has a small mouth and that there is not enough room for all their teeth, the therapist would then refer the child to an airway centric dentist or orthodontist. The parent may also tell the therapist that the child is constipated and only poops once every 7 to 10 days, this would require a referral to a GI doctor. So, the child who came in with the chief complaint of speech and feeding problems has a list of issues that the parent had no idea were related.
It is very uncommon that one professional will help improve the child’s overall functioning. This is why if a child has oral motor dysfunction, the best place to start is with a speech and language pathologist. A functional evaluation by a speech and language pathologist with oral motor training will help parents better understand what the problem is, what the problem could be related to, and will be able to create a treatment plan for overall wellness and functioning.